Diffuse large B-cell lymphoma: What you need to know about diagnosis and treatments
Diffuse large B-cell lymphoma, or DLBCL, is the most common type of non-Hodgkin lymphoma (NHL), accounting for more than 30 percent of all cases. While it is considered an aggressive type of lymphoma, it also is potentially curable for many patients — especially now that treatments are becoming more targeted, more specific and more personalized.
What is diffuse large B-cell lymphoma (DLBCL)?
DLBCL is a cancer of white blood cells called B lymphocytes. It begins when these B lymphocytes grow uncontrollably, enlarging the lymph nodes and sometimes traveling to other organs, such as the bone marrow, spleen and liver. Symptoms often include night sweats, weight loss and fatigue.
How is DLBCL diagnosed?
The first step to confirming a DLBCL diagnosis is to look at the cells under a microscope with a biopsy. DLBCL has many different biologic variants and requires expert pathologists to determine the exact variant. After this, special stains, a test called flow cytometry, and a study of the chromosomes give us more information about the biology of the cells. Finally, we want to know how much lymphoma is present in the patient, so we do a PET or PET-CT scan to tell us where it is located and how metabolically active it is. All this leads to a prognosis and a treatment plan based on the disease type and other factors, such as the patient’s age and overall health.
New tools, such as genetic tests, can give us more information about what subtype of DLBCL is present. This is helpful in understanding more about how a patient will respond to a particular treatment and is leading to more individualized therapies for the different subtypes.
What is the standard of care for DLBCL?
As with many blood cancers, the first line treatment for DLBCL is chemotherapy. In most cases, patients receive a combination of five medications, known as R-CHOP.
R-CHOP, or other more intense treatment combinations, is often successful in curing DLBCL. However, if the cancer comes back, we have other options, including additional chemotherapy and autologous (using the patient’s own cells) stem cell transplant. The sequence and amount of each additional therapy depends on the aggressiveness of the cancer and the patient’s response to the therapy.
What treatments are available for relapsed DLBCL?
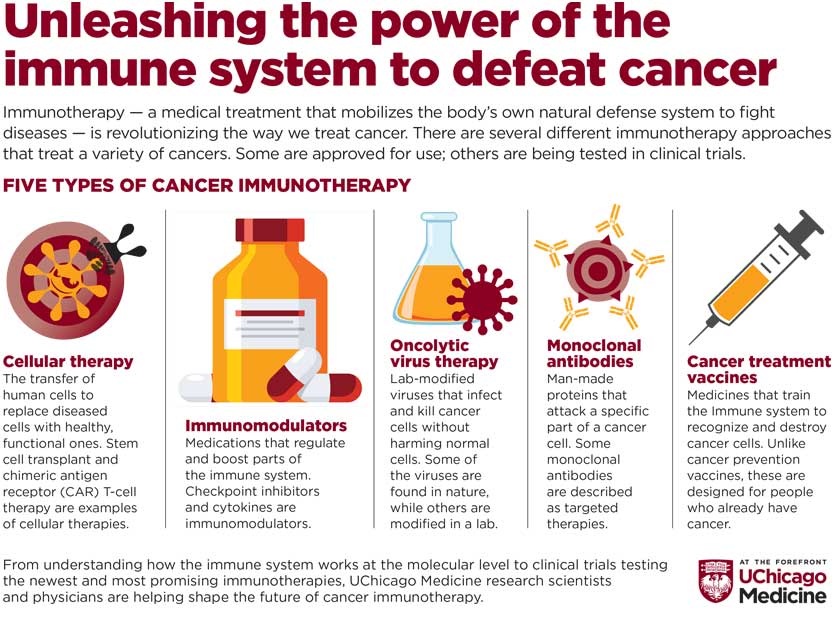
If a patient isn’t cured after chemotherapy and stem cell transplant, we have several different options. In fact, it’s an incredible time when it comes to new drugs and new therapies. In 2019 and 2020 alone, three new treatments were approved for use in relapsed and refractory DLBCL. Examples are antibody-drug conjugates, which are antibodies linked to a “trojan horse” delivery of an anti-cancer drug; oral pathway inhibitors, which selectively block some of the pathways that lymphoma uses to grow; and a new antibody against a common protein on cancerous B-cells. There is also the new field of immunotherapy, where the drugs affect or block how the immune system recognizes cancer. CAR T-cell therapy, an immunotherapy that has had a lot of attention in the medical community and the media in the past several years, has been a game-changer for many patients with DLBCL and other blood cancers.
Read about two patients with relapsed lymphoma who participated in clinical trials testing immunotherapies for DLBCL.
What do you see on the horizon for patients with DLBCL?
Treatment for lymphoma will become more targeted, more personalized and more specific to each patient and their disease. And by analyzing a tumor we can understand its biology and select optimal treatments while minimizing any toxicities of the medications. View clinical trials of new treatments for lymphoma.

Sonali M. Smith, MD
Sonali M. Smith, MD, is an expert in lymphoma care and research and is the Chief of the Section of Hematology/Oncology. Dr. Smith is actively researching new treatments for lymphoma, such as immunotherapies that harness the body's immune system to fight cancer.
Learn more about Dr. Smith
Sickness is relentless. So are we.
We are a leading community of physicians, researchers and game changers. We embrace challenges and turn them into opportunities to make a difference in your life.
Learn more about UChicago Medicine's undaunted approach to care.
